The COVID-19 outbreak continues to dominate our everyday lives, with the Movement Control Order (MCO) announced on March 16 severely restricting our capacity to carry out tasks that, until so recently, seemed commonplace and mundane. With Malaysians now spending their days at home, the media machine, both mainstream and social, has gone into overdrive, leading to voracious consumption and republication of anything Covid-19 related.
Among the news articles that have held our attention since the MCO came into force are the reports concerning individuals suspected of being infected by the virus, or of having come into contact with others who tested positive, who are reluctant to come forward to be tested themselves.
This scenario, playing out in real time in front of our eyes, raises an important and very real question — can a person suspected of being infected with the Covid-19 virus, or someone who has had contact with an infected person, be compelled to be tested for the virus despite his reluctance or outright refusal?
Common law jurisdictions have long recognised the right of patients to refuse to accept medical treatment, even to their own obvious detriment. Consider the example of a patient with a tumour who refuses to undergo a biopsy to ascertain whether it is benign or cancerous. In this situation, the law will not step in to compel the patient to test for cancer or to subsequently receive treatment - even if this choice could potentially lead to the patient’s death.
In Airedale NHS Trust v Bland [1993] 1 All ER 821, the UK Court of Appeal held up the principle of patient autonomy in respect of decisions affecting their own health as “paramount”. The Court explained that if a patient is capable of making a decision on whether to undergo treatment, their decision to refuse such treatment must be obeyed even if, on an objective view, that decision is contrary to their own interests.
However, the principles of self-determination and autonomy do not lend themselves well in dealing with the pandemic that currently faces the world. Individuals asserting their right to refuse treatment by declining to be screened for the Covid-19 virus would be behaving in a manner contrary to the collective, urgent need for the virus to be contained and eradicated.
This clash of principles was discussed by the Ontario Court of Appeal in Malette v. Shulman (Ont. C.A.), 72 O.R. (2d) 417. In its judgment, the Court observed that there are circumstances where the individual's right to self-determination may be overridden, such as where citizens are required to submit to medical procedures in order to “eliminate a health threat to the community”.
In Malaysia, such an exception to the individual’s right to refuse medical treatment is codified in the Prevention and Control of Infectious Diseases Act 1988 (PCID). The current MCO was issued under the PCID as well as the Police Act 1987.
There are two provisions of the PCID which are particularly relevant to this discussion.
Section 11 of the PCID empowers “authorised officers” to direct any person living in an “infected local area” to subject themselves to “treatment” or “immunisation”, or to “isolation”, “observation” or “surveillance” for a specified period of time.
Section 15 of the PCID allows an officer to order any contact to undergo “observation” or “surveillance” until they may be discharged without danger to the public.
There are a few things to note with regard to the terms used in the PCID:
(a) the phrase “authorised officer” is defined rather widely, and includes any medical practitioner in the service of the government as well as any local authority carrying out the duty of a medical officer;
(b) all states and Federal Territories in Malaysia were declared “infected local areas” under the Prevention and Control of Infectious Diseases (Declaration of Infected Local Areas) Order 2020 gazetted on March 17, 2020;
(c) “treatment” includes any act necessary to determine whether a person is infected with an infectious disease; and
(d) “observation” is defined as the segregation of any person to ascertain whether they are suffering from an infectious disease and includes treatment.
Taking these factors in their totality, an authorized officer, including a doctor in the government sector, can compel an individual, whether one suspected of being infected or of having close contact with someone infected, to undergo screening for the Covid-19 virus during the continued enforcement of the MCO.
Pertinently, in the event the individual is uncooperative and refuses to comply with an order to undergo screening, the authorized officer is allowed to use force or such methods as may be necessary to ensure that the individual undergoes the screening — this could include obtaining the aid of police officers to ensure compliance. Additionally, non-compliance with such a directive is an offence under the PCID and is punishable by imprisonment for a term not exceeding two years or by a fine (or both) for a first offender.
We are already seeing these provisions being enforced. Since the MCO came into effect on March 18, there have been reports of individuals refusing to cooperate with its prescriptions. These include a report of an incident in Labuan, where an individual refused to undergo screening for the Covid-19 virus, despite having come into contact with a person under investigation for the virus. According to the reports, the police were called in to ensure that the individual underwent screening and complied with the required 14-day quarantine.
The provisions in the PCID which allow authorized officers to compel Covid-19 screening are not unique to Malaysia. In the United Kingdom, under the Public Health (Control of Disease) Act 1984, an order may be made that requires a person to submit to a medical examination, or be removed or detained in a hospital or kept in quarantine. The Health Protection (Coronavirus) Regulations 2020, issued pursuant to the 1984 Act, provide specific provision for detaining individuals for the purpose of Covid-19 screening if there are reasonable grounds to believe that a person is infected by the virus or if the person had visited an infected area within the previous 14 days.
Across the causeway, Singapore’s Infectious Diseases Act 1976 empowers the authorities to require any person who is, or is suspected to be, a case or carrier or contact of an infectious disease to submit to a medical examination or to medical treatment. In 2017, the Singapore Ministry of Health ordered a man to undergo testing for HIV and subsequently prosecuted him for, among others, failing to undergo the necessary tests to ascertain whether he was HIV positive before engaging in sexual activity, despite having reason to believe that he was infected, and failing to inform his partner of the risk of contracting HIV from him.
It is worth noting that medical practitioners in private practice do not have the authority to compel a patient to undergo testing for Covid-19. On this front, the Ministry of Health has issued the Covid-19 Management Guidelines No.5/20, containing advice for private healthcare providers. The guidelines advise private clinics and private hospitals to provide visual signage requesting patients to declare symptoms, travel or contact with a confirmed case. It also provides advice on how to triage patients and gives direction on the circumstances in which patients ought to be referred to government health centers for screening or admission. Clearly, healthcare providers will need to be vigilant and exercise a high index of suspicion in these extraordinary times.
Moving forward, the provisions of the PCID may be invoked to compel Covid-19 screening for reluctant members of our society who meet the prescribed MOH criteria. Ultimately, while the principles of self-determination and the autonomy of the individual patient are generally held up as inviolate, these are exceptional times which require exceptional measures. The threat to society as a whole and to its individual members cannot be ignored and must be taken as paramount now and in the coming weeks of this battle against the Covid-19 pandemic.
Raja Eileen Soraya, Harish Nair and Latifa Haiqa Yusoff are advocates and solicitors of the High Court of Malaya.
Stay calm. Stay at home. Keep updated on the latest news at www.EdgeProp.my #stayathome #flattenthecurve
TOP PICKS BY EDGEPROP

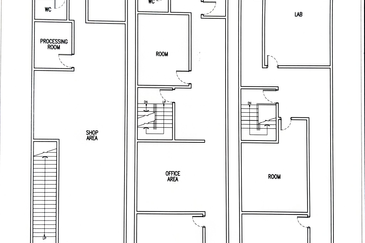
Kawasan Perindustrian MIEL
Batang Kali, Selangor

Livia @ Bandar Rimbayu
Telok Panglima Garang, Selangor

Robin @ Bandar Rimbayu
Telok Panglima Garang, Selangor

Penduline @ Bandar Rimbayu
Telok Panglima Garang, Selangor

Penduline @ Bandar Rimbayu
Telok Panglima Garang, Selangor

Chimes @ Bandar Rimbayu
Telok Panglima Garang, Selangor

Taman Tun Dr Ismail (TTDI)
Taman Tun Dr Ismail, Kuala Lumpur